40 is the New 50: What New Colon Cancer Screening Guidelines Mean to You
Colon cancer screening is an essential part of living a healthy lifestyle and can be lifesaving. Colorectal cancer, worldwide, is the second leading cause of cancer death, according to Cancer.Net. There is no one-size-fits-all rule when it comes to health screenings; however, new guidelines for colon cancer are available. Discover how the recent colon cancer screening guidelines may affect you.
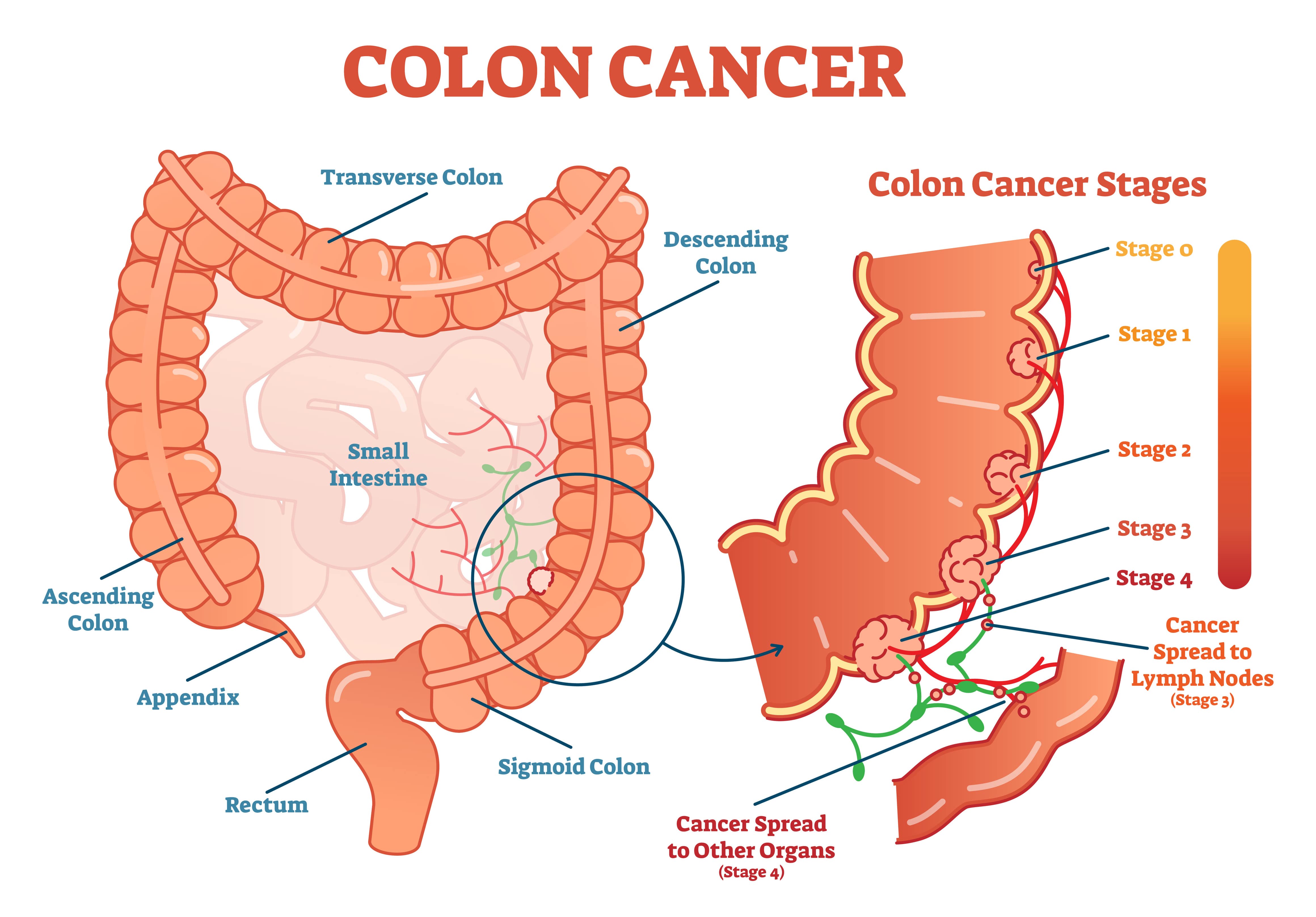
What Is Colon Cancer?
Colon cancer is often called colorectal cancer because this cancer starts in the colon or the rectum. The cancer is called colon cancer if cancer begins in the colon and rectal cancer if it starts in the rectum.
Colorectal cancer is a disease where abnormal growths called polyps form in the colon or rectum. Gradually, these polyps may turn into cancer. Polyps come in different types with different risks of colon cancer. If these are found during your colonoscopy, your physician will remove these polyps for biopsy. The frequency of your screening colonoscopies will depend on the number of polyps, the size of the polyps, and the type of polyp under microscopy in addition to other risk factors related to your medical and family history.
Colon Cancer Symptoms
Symptoms of colorectal cancer often do not show up until the later stages of the disease. Colorectal cancer symptoms include red streaks of blood in the stool, diarrhea or constipation, bloating, and abdominal pain. Rectal bleeding, blood in the toilet after bowel movements, and dark or black stools are symptoms. A feeling of needing to have a bowel movement when the bowel is empty could signal colorectal cancer. Unexplained weight loss and fatigue are common colorectal cancer symptoms.
Risk Factors
Risk factors for colorectal cancer are not always within a person’s control, but some lifestyle factors help cut risk. The factors out of an individual’s control are those with a family history of colorectal cancer, and individuals with a history of chronic inflammatory diseases. Lifestyle choices that can cut the risk of colorectal cancer are quitting smoking, not drinking alcohol, eating a low-fat, high-fiber diet as well as getting exercise.
Colorectal Cancer Diagnosis
Diagnosis of colorectal cancer has many forms. The most common forms of colon cancer screening are:
Stool Tests
Polyps and colorectal cancers can bleed. Stool tests check for small amounts of blood in feces. Blood in stools may not always be accurate because blood may come from non-cancerous sources such as hemorrhoids. Colonoscopy is often necessary after blood is found in stool to find and remove polyps.
Sigmoidoscopy
The sigmoidoscope is a flexible, lighted tube with a lens to examine the rectum and sigmoid colon. There is a tool for removing tissue such as polyps. The sigmoid colon is the last section of the colon that attaches to the rectum. A sigmoidoscopy is not a full colon survey.
Colonoscopy
A colonoscopy looks at the entire colon and rectum using a flexible, lighted tube, a colonoscope with a viewing lens, and a tool for removing tissue. Like a sigmoidoscopy, a colonoscopy requires emptying the bowels in preparation for clear viewing of the area. A colonoscopy, unlike a sigmoidoscopy, requires sedation.
Virtual Colonoscopy or Computed Tomographic (CT) Colonography
CT uses special x-ray equipment (a CT scanner) for colon cancer screening to produce pictures of the colon and the rectum without using a colonoscope. The disadvantage of virtual colonoscopy is if polyps are discovered, the physician can’t immediately remove the polyps and will need to use colonoscope surgery to remove polyps.
New Screening Guidelines
The U.S. Preventive Services Task Force (USPSTF) has updated its guidelines to begin colon cancer screening at age 45 because more people, according to USPSTF statistics, are developing colorectal cancer under 50 years of age. Recommended intervals are:
-
- High-sensitivity stool blood gFOBT or FIT test every year.
- SDNA-FIT stool blood test every one to three years.
- CT (virtual colonoscopy) colonography every five years.
- Flexible sigmoidoscopy every five years.
- Flexible sigmoidoscopy every ten years and FIT stool blood test every year.
- Colonoscopy screening every ten years.
People with polyp findings and removal or other risk factors may have more frequent colon cancer screening because these factors put people in higher-risk categories for developing colorectal cancer. For example, the American College of Gastroenterology recommends screening at age 40 for people with one or two first-degree relatives with colorectal cancer or advanced colorectal polyps.
Why Earlier Colon Cancer Screening is Important
According to a study in the journal Cancer Epidemiology, Biomarkers & Prevention, early-onset colorectal cancers are becoming more common in young people between 20 and 39 years. The increase appears more pronounced in Black and Hispanic populations.
Early-onset colorectal cancer is cancer in patients younger than 50 years old, and the biggest increases were in later-stage colorectal adenocarcinomas. There was a 48-percent increase from 2000 to 2016 in later-stage rectal adenocarcinomas in patients 30-39 years old, and a 133-percent increase for same cancer in patients aged 20-29 years. Black and Hispanic people had the most significant cancer increase, with rates more than double for some colorectal cancers. Earlier colon cancer screening can help save lives, especially in higher-risk categories.